Tiroides De Hashimoto, also known as Hashimoto’s thyroiditis, is an autoimmune disease affecting the thyroid gland. This condition, characterized by the body’s immune system mistakenly attacking the thyroid, impacts millions worldwide, leading to a range of symptoms and potential long-term health consequences. Understanding the nuances of this disorder, from diagnosis to management, is crucial for effective treatment and improved patient outcomes.
This pervasive autoimmune disorder primarily affects women and can manifest with symptoms ranging from fatigue and weight gain to depression and infertility. Early diagnosis and appropriate management are vital to mitigate potential complications and improve quality of life. This article delves into the complexities of Hashimoto’s thyroiditis, exploring its causes, symptoms, diagnosis, treatment options, and the importance of lifestyle modifications.
Hashimoto’s Thyroiditis: A Comprehensive Overview: Tiroides De Hashimoto
Hashimoto’s thyroiditis, also known as chronic lymphocytic thyroiditis, is an autoimmune disease affecting the thyroid gland. This condition leads to hypothyroidism, a state where the thyroid doesn’t produce enough thyroid hormones. Understanding its nature, diagnosis, treatment, and potential complications is crucial for effective management and improved patient outcomes.
Hashimoto’s Thyroiditis: An Overview
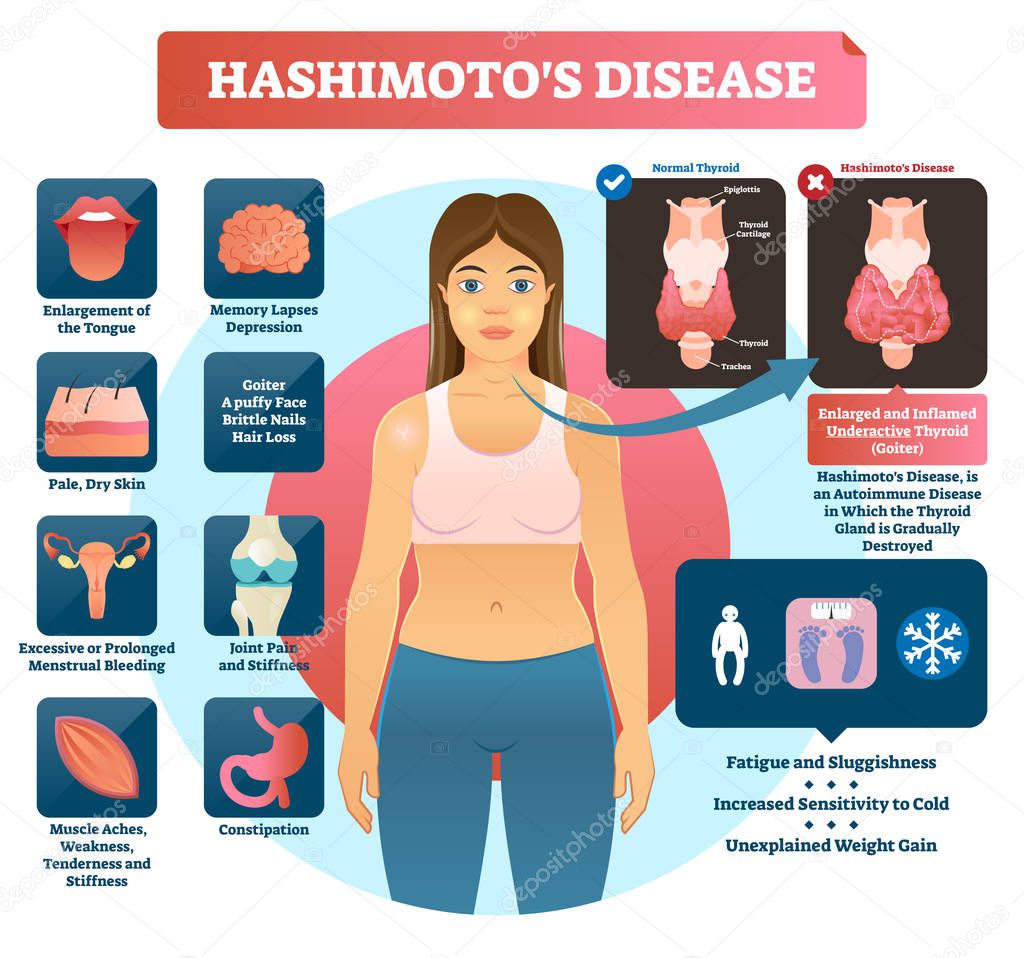
Hashimoto’s thyroiditis is characterized by the body’s immune system mistakenly attacking the thyroid gland. This autoimmune response causes inflammation and gradual destruction of thyroid tissue, reducing its ability to produce essential hormones like thyroxine (T4) and triiodothyronine (T3). The prevalence of Hashimoto’s is higher in women, typically manifesting between the ages of 30 and 50, although it can occur at any age.
Symptoms can range from subtle to severe, varying significantly among individuals.
Typical Symptoms of Hashimoto’s Thyroiditis
Many individuals with Hashimoto’s experience a gradual onset of symptoms, often going unnoticed for extended periods. Common symptoms include fatigue, weight gain, constipation, dry skin, cold intolerance, muscle aches, depression, and cognitive impairment. In some cases, a goiter (enlarged thyroid gland) may be palpable. It’s important to note that symptom severity can vary considerably.
Comparison of Hashimoto’s Thyroiditis with Other Thyroid Conditions
Differentiating Hashimoto’s from other thyroid conditions is crucial for accurate diagnosis and appropriate treatment. The following table highlights key distinctions:
| Feature | Hashimoto’s Thyroiditis | Graves’ Disease | Hypothyroidism (Non-autoimmune) |
|---|---|---|---|
| Autoimmune Basis | Yes | Yes | No |
| Thyroid Hormone Levels | Low (hypothyroidism) | High (hyperthyroidism) | Low (hypothyroidism) |
| Goiter | Often present | Often present | May or may not be present |
| Treatment | Hormone replacement therapy | Antithyroid drugs, radioactive iodine, surgery | Hormone replacement therapy (if needed) |
Diagnosis and Testing Procedures
Diagnosing Hashimoto’s typically involves a combination of blood tests and imaging studies. Early detection is crucial to prevent long-term complications.
Blood Tests for Hashimoto’s Thyroiditis
The primary blood tests used to diagnose Hashimoto’s include thyroid-stimulating hormone (TSH), free thyroxine (FT4), and free triiodothyronine (FT3). Elevated TSH levels along with low FT4 and FT3 often indicate hypothyroidism. Additionally, thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb) are often tested to confirm the autoimmune nature of the condition. High levels of these antibodies strongly suggest Hashimoto’s thyroiditis.
Role of Thyroid Ultrasound in Diagnosis
A thyroid ultrasound can visualize the thyroid gland, assessing its size, shape, and texture. This imaging technique helps detect the presence of a goiter and identify any nodules or irregularities within the thyroid tissue. While not diagnostic on its own, it provides valuable supplementary information to blood test results.
Challenges in Diagnosing Hashimoto’s Thyroiditis
Diagnosing Hashimoto’s can sometimes be challenging due to the variability in symptoms and the possibility of subclinical hypothyroidism (slightly low thyroid hormone levels without overt symptoms). Furthermore, overlapping symptoms with other conditions can complicate the diagnostic process.
Step-by-Step Diagnostic Process
- Initial consultation with a physician, reviewing symptoms and medical history.
- Blood tests to measure TSH, FT4, FT3, TPOAb, and TgAb.
- Thyroid ultrasound to visualize the thyroid gland.
- Review of test results and potential further investigations if needed.
- Diagnosis and discussion of treatment options.
Treatment Options and Management Strategies
The primary treatment for hypothyroidism caused by Hashimoto’s is hormone replacement therapy (HRT). This involves supplementing the missing thyroid hormones to restore normal thyroid function.
Hormone Replacement Therapy (HRT)
HRT aims to replace the deficient thyroid hormones with synthetic versions, typically levothyroxine (T4). The dosage is carefully adjusted based on individual needs and monitored through regular blood tests. The goal is to achieve normal TSH, FT4, and FT3 levels.
Types of Thyroid Hormone Replacement Medications
Levothyroxine (Synthroid, Levoxyl, others) is the most commonly prescribed medication for hypothyroidism. In some cases, a combination of levothyroxine and liothyronine (T3) may be considered, though levothyroxine alone is usually sufficient. The choice of medication and dosage depends on individual patient factors and response to therapy.
Sample Treatment Plan for Hashimoto’s Thyroiditis
| Stage | Action | Monitoring | Duration |
|---|---|---|---|
| Initial Assessment | Comprehensive medical history, physical examination, blood tests (TSH, FT4, FT3, TPOAb, TgAb), thyroid ultrasound. | Symptoms, weight, mood. | 1-2 weeks |
| Levothyroxine Initiation | Start levothyroxine at a low dose. | TSH, FT4 levels after 6-8 weeks. | Ongoing |
| Dosage Adjustment | Adjust levothyroxine dose based on TSH and FT4 levels. | TSH, FT4 levels every 6-8 weeks until optimal levels are achieved. | Ongoing |
| Long-term Monitoring | Regular blood tests to monitor TSH, FT4, and FT3 levels. | Symptoms, weight, mood, and overall well-being. | Ongoing |
Lifestyle Factors and Dietary Considerations
Maintaining a healthy lifestyle plays a significant role in managing Hashimoto’s thyroiditis. Diet and stress management are particularly important aspects.
Hashimoto’s Thyroiditis, or Tiroides De Hashimoto, is a common autoimmune disorder affecting the thyroid gland. Managing this condition often requires regular monitoring of thyroid hormone levels, and convenient access to test results is crucial. Patients can access their health information, including thyroid test results, through the BayCare patient portal; for example, you can find information on how to log in at the patient portal baycare website.
Proactive management via this portal empowers individuals with Hashimoto’s to actively participate in their healthcare journey.
Diet and Thyroid Health
A balanced diet rich in fruits, vegetables, whole grains, and lean protein is essential. Foods rich in iodine, such as iodized salt, are important for thyroid hormone production, but excessive iodine intake should be avoided. Some individuals report improvements with a gluten-free diet, although this isn’t universally effective. Cruciferous vegetables (broccoli, cauliflower, cabbage) have been associated with potential interference with thyroid hormone production in some individuals, but this effect is generally minimal unless consumed in very large quantities.
Stress Management Techniques
Stress can exacerbate autoimmune conditions, including Hashimoto’s. Practicing stress-reducing techniques, such as yoga, meditation, deep breathing exercises, and regular physical activity, is highly beneficial for overall well-being and managing Hashimoto’s symptoms.
Potential Complications and Long-Term Effects, Tiroides De Hashimoto
Untreated or poorly managed Hashimoto’s can lead to various complications. These complications can range from mild to severe, impacting various aspects of health.
Long-Term Complications of Untreated Hashimoto’s
- Severe hypothyroidism: leading to significant fatigue, weight gain, cognitive impairment, and other symptoms.
- Cardiovascular issues: increased risk of heart disease due to high cholesterol and other factors.
- Infertility and pregnancy complications: hypothyroidism can affect fertility and increase the risk of miscarriage.
- Goiter: enlarged thyroid gland that can cause discomfort and cosmetic concerns.
- Myxedema coma: a rare but life-threatening complication of severe hypothyroidism.
Hashimoto’s and Other Autoimmune Diseases
Individuals with Hashimoto’s have a higher risk of developing other autoimmune diseases, such as type 1 diabetes, rheumatoid arthritis, and celiac disease. This highlights the importance of regular health check-ups and monitoring for other potential autoimmune conditions.
Illustrative Case Studies
Source: depositphotos.com
A 45-year-old woman presented with complaints of persistent fatigue, weight gain, constipation, and cold intolerance for the past six months. She also reported experiencing difficulty concentrating and experiencing mood swings. Blood tests revealed elevated TSH levels and low FT4 and FT3, along with high TPOAb and TgAb. A thyroid ultrasound showed a slightly enlarged thyroid gland. The diagnosis of Hashimoto’s thyroiditis was made, and she was started on levothyroxine.
After several months of treatment and dosage adjustments, her symptoms improved significantly, and her thyroid hormone levels normalized. She continues to monitor her health and maintains a balanced diet and stress management techniques to support her overall well-being. Her long-term prognosis is excellent with continued hormone replacement therapy and lifestyle adjustments.
Closing Notes
Hashimoto’s thyroiditis, while a significant health concern, is manageable with proper diagnosis and treatment. Understanding the autoimmune nature of the disease, along with proactive lifestyle changes and adherence to medical advice, empowers individuals to navigate this condition and maintain a healthy, fulfilling life. Early detection and consistent monitoring are key to preventing long-term complications and ensuring optimal well-being.
